But for McNair and other mental-health professionals, the division closure itself isn't the most disconcerting element of MSH's decision to do away with its community-based care. Photo by Trip Burns.
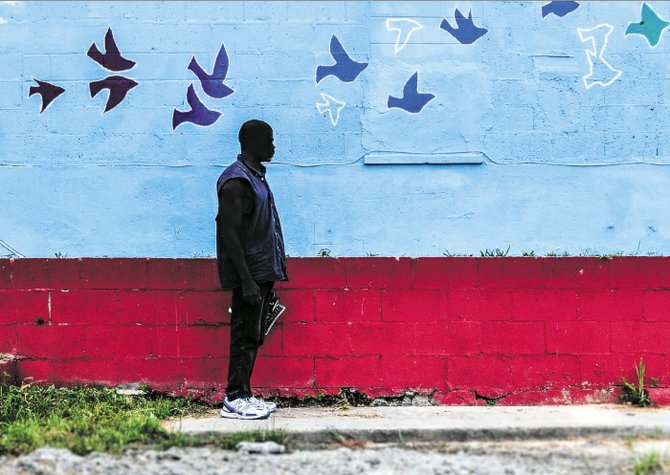
When Joe Adams talks, his words leave his mouth so quickly they fall over themselves, but he doesn't appear frantic. The wrinkles on his face, around his eyes, fold and overlap as his expression changes. His scratchy golden goatee surrounds a warm, closed-lip smile when he's listening.
The tips of his index finger and thumb are burnt black. He said it's from smoking down his cigarettes too far. "I've got a pretty bad cigarette habit," Adams said.
It's almost as bad as his coffee habit—but smoking cigarettes and drinking coffee are the way most mentally ill and homeless people like him get by. Adams isn't living in a shelter right now. Instead, he spends his days at the Opportunity Center in downtown Jackson and his nights on the street.
"I've been staying outside for a while. I've been enjoying it. You know you can't smoke cigarettes and drink coffee in there," Adams said of the homeless shelter. "So I've been enjoying it outside."
He's been diagnosed, as he said, with paranoid schizophrenia and depression. He is able to get medication from the Opportunity Center director, Christie Burnett. Doctors from St. Dominic Hospital told Adams after the last time he was admitted there that the medication is working.
Adams has been institutionalized more than three times, including at Mississippi State Hospital at Whitfield, an inpatient mental-health hospital, but he doesn't need to be. It is better for Adams to be part of a community, like the one at the Opportunity Center, where he interacts all day with the staff and other homeless people there. He said his days partly consist of playing basketball and lifting the bricks outside like weights.
"I eat lunch. I smoke cigarettes. I'm waiting on a lawyer to get my compensation—my mental health check, my SSI (Supplemental Security Income)—and Mrs. Christie is helping me get my food stamps. I'll eat lunch. I'll stay here. I'll drink the coffee, talk to people here, smoke cigarettes outside, play cards, read the books," Adams said.
The other homeless people who receive checks offer Adams cigarettes and coffee when he's out. "There's decent people here," he said. But he needs more.
In fact, Burnett said, the medications Adams is receiving are "nothing compared to what he needs," suggesting he'd be a lot better off in a case-management program and with additional community services. Unfortunately for Adams and the many people in his situation, mental-health services for people living in the community are lacking in the state of Mississippi.
Burnett said Adams was again institutionalized at MSH on Aug. 26, a few weeks after he spoke to the JFP.
Adams said he has never lived in group home or participated in community-based mental-health services. "I'd like to. I'd love to do that," he said. Adams said doctors from St. Dominic never told him about community-based services—just told him to take his medication. Like most people in his situation, Adams had been referred to Hinds Behavioral Health Services—an outpatient mental health clinic—but getting to its location in west Jackson is difficult for people like Adams.
"I didn't make it to Hinds Behavioral. I didn't have a ride," Adams said. "All I knew was what they told me at St. Dominic when I left."
A Vacant Campus
Adams' eyes lit up when told about Mississippi State Hospital's Community Services Division, which provided community-based patients mental-health care, drop-in appointments, and even a place for homeless people to bathe and wash clothes. He didn't know about it. The light in his face faded when he learned the program closed May 1, 2014. MSH and the Department of Mental Health decided to close the program after a deficit in funds.
Just a few blocks from the Opportunity Center and in walking distance from an area of town where many homeless people congregate, a campus of abandoned buildings withers away. Its only occupant is a lone security guard who deters trespassers. The brick buildings probably didn't look any nicer when they were inhabited by patients, but the overgrown grass and empty parking lot tell a story of 120 people suffering from mental illness who were stripped of essential services.
Since 1986, MSH Community Services served mentally ill members of the community who didn't need to be institutionalized with outpatient care including case management, counseling, rehabilitation, and access to laundry and bathing facilities.
The Community Services Division had buildings in downtown Jackson in close proximity to the Stewpot and the Opportunity Center—two facilities that help feed and provide services to the homeless community. A case-management program called Project for Assistance and Transition from Homelessness (PATH) operated in what was called the Jimmy Stubbs House located at 350 Capers Ave. and offered extensive outreach to the homeless and mentally ill community.
The division also operated Community Living Services, consisting of two group homes—Villa Hope and Crossroads—and a transitional rehabilitation home called the Mental Illness and Chemically Addicted Recovery Environment (MICARE).
Hard to Swallow
In 2013, MSH decided, with help from the Mississippi Department of Mental Health, to close their community-based services and prioritize their acute inpatient care at Whitfield. Lynn McNair, longtime mental-health advocate and former director of Mental Health Association of the Capital Area, doesn't quite buy this explanation.
"The Community Services Division of Mississippi State Hospital has been in existence for 30 years. All of a sudden, they decided that their primary focus all along had been acute care for people in the hospital. But these services had been in place for 30 years, so it's a little hard to swallow. This is about money," McNair said.
The decision came after a decrease in funds in recent years, including legislative budget slashes in appropriation bills over a six year period. DMH cited the budget cuts as a motivator behind prioritizing acute inpatient care at MSH over community-based care, like the care provided at the Capers Avenue location. MSH and DMH claim the closure allows them to operate within their current financial means and focus funds on inpatient care. Ultimately, hospital officials claim community services were never in line with the mission of the facility.
But for McNair and other mental-health professionals, the division closure itself isn't the most disconcerting element of MSH's decision to do away with its community-based care.
"My biggest concern is: Where are the 120 people that were in the program?" McNair said.
Not even the Department of Mental Health knows exactly where all of the mentally ill patients who were using MSH's Community Services have gone since the closure. This is why McNair filed a complaint with an agency called PEER (Performance Evaluation Expenditure Review), which conducts investigations and publishes reports. Working with the agency is the Joint Legislative Committee on PEER made up of Mississippi legislators—seven representatives and seven senators.
Falling Through the Cracks
Throughout PEER's investigation, the agency found that "MSH could not readily determine where clients" from MSH Community Services "were located or where they were going."
Julia Weems, who was a social worker at St. Dominic's Behavioral Health until July, witnessed mentally ill patients who "fell through the cracks" due to the Community Services closure. St. Dominic began to admit patients they had never even seen before—adults with severe mental illness they had no history with. It was clear to Weems that MSH at Whitfield served patients who were using MSH's Community Services when they became ill, saying that MSH's "service delivery was kind of insular." But the closure forced them to find other providers.
MSH apparently transferred the patients who were living in Community Services group homes—around 13 patients according to the PEER report—to personal-care homes in the area. While MSH provided health services to patients in its Community Living Services program, those patients would have to find a new provider once they were in a personal-care home, but the transition has not been easy.
"We definitely saw cases of people who had been transferred from the group homes to various personal-care homes around the city who just fell apart, who just decompensated because they had been doing well and were stable for many years in the situation they were in," Weems said.
An environmental transition like this, Weems said, is exceptionally difficult for a person suffering mental illness. "I don't know what kind of follow-up services or transitional support these folks had," Weems said.
One patient in particular, who was let go from Community Services, had such a difficult transition that when he ended up in the care of Weems, he couldn't communicate where he was from, his background, his health history or any of his family's contact information. After a while he was able to get Weems in touch with his mother.
"The poor woman had no idea where he was for a month. She had been contacted by somebody at State Hospital saying they were moving him to a different group home. She said nobody ever followed up with her to tell her where he went," Weems said.
Weems found it extremely disconcerting that this man's mother did not know where her mentally ill son was. Weems doesn't claim that what MSH did to their patients was as extreme as "throw people to the streets"—as some mental-health advocates have suggested. Still, she is concerned that vulnerable adults are not fully protected.
"I don't understand how they negotiated this transition, how they planned for the ease of transition for these people who were dependent on them—who needed protection, who needed extra support. Not to mention the burden that the closure of Community Services has placed on Hinds Behavioral Health," Weems said.
Ophelia Kelly, director of treatment services at Hind Behavioral Health Services, told the Jackson Free Press that they received approximately 100 patients from MSH Community Services. Kelly claims the influx has not put a great burden on Hinds Behavioral, since taking in new patients is what they do on a normal basis. Hinds Behavioral Special Projects Director Kahne Simmons confirmed this.
"It's not a new function for us it's just been a (greater) case load," Simmons said.
Weems, however, disagreed. "I've talked to people who work there who have talked to me anecdotally about how hard it is to work all these folks into case management and to intake. They're already overburdened," Weems said. She wasn't surprised that Hinds Behavioral officials would try to put the situation in a more optimistic light than it deserves.
Rep. Becky Currie, R-Brookhaven, who is on the PEER committee, said the DMH has a sort of hold over the community mental-health centers, like Hinds Behavioral.
"The community mental health is under their thumb—they're adversaries and they don't get along. The Department of Mental Health have their thumb on the community mental health's money," Currie said.
Additionally, Hinds Behavioral is located on U.S. Highway 80 in west Jackson, which makes appointments there inconvenient for people who normally received services in their immediate communities, especially homeless clients who used the Jimmy Stubbs House, which is just off West Capital St. near Stewpot. Just because Hinds Behavioral received patients from Community Services—half of which Kelly said did not come with medical history, does not mean they are receiving services from them as often as they did from Community Services.
Heather Ivery, director of business administration at Stewpot, expressed concerns over patients' inability to go to Hinds Behavioral or other outpatient facilities. For people facing mental illness, changing doctors is a huge change.
"You can refer somebody anywhere, but if they're in this mental state already, a lot of times they're not trusting. You know, change is never easy, and if you already have a mental illness on top of that, change can be real difficult.
"So whether or not these clients—even that I've talked to that say they've been referred—are going to go to Hinds Behavioral is a whole other ball game," Ivery said.
Shut the Doors
MSH spokesman Adam Moore declined to set up interviews with MSH officials for this story, but emailed a statement stating that other community-based care providers are serving all community-based patients and that "MSH transition coordinators will track each individual for one year to ensure continuity of services and transition to new service providers."
However, the PEER report states that MSH has no system in place to track patients to see that they have been transferred to other providers smoothly.
Maria Hamblin, executive director at My Father's House of Freedom, said a phone call was the extent of MSH's tracking of her clients—all of whom were Community Services patients.
"I did receive a phone call from someone there that I had not worked with before just wanting to make sure that the clients had gone on to get services, but that's been all for that," Hamblin said.
My Father's House is a transitional home for those suffering substance abuse, many of whom got involved in drugs and alcohol due to their mental illness. Fortunately for the eight to 10 Father's House clients discharged from Community Services, Hamblin collaborated with Community Services to help choose their new provider and facilitate their transfer to either Hinds Behavioral or Mission First in Jackson.
Still, the transition has not been easy. "It's been a great loss for us," Hamblin said. She also said the fees that Hinds Behavioral charges have created an issue for her and her clients.
Hamblin did say the hospital has been helpful in facilitating the transfer for her clients, but that there is "not a real good alternative for the type of care they were getting there, which was very good," Hamblin said of Community Services.
"It's like they just shut the doors, and that was it," Weems said.
Out of Compliance
MSH and DMH also claim that the state hospital only began the Community Services Division 30 years ago because no one else was providing community-based care in the area and that redirecting their resources to inpatient care was the best use of their funds presently.
But under the Americans with Disabilities Act (ADA) of 1990, the state has an obligation to serve mentally ill members of the community with services in the most integrated setting possible. That is, they are not to institutionalize patients unless it is absolutely necessary. In the 1999 U.S. Supreme Court decision Olmstead v. L.C., the court determined that inappropriate institutionalization of mentally ill patients, who could be participating in the community, constitutes discrimination under Title II of ADA.
Christy Dunaway, director of Living Independence for Everyone (LIFE), said this is the crucial court decision in determining how to treat mentally ill patients.
"Olmstead focuses more on the state, so it's the state that is obligated to have more home and community services—of course, it's the state hospital at Whitfield," Dunaway said.
In this way, Olmstead puts a greater responsibility on the state hospital to provide community services. Dunaway said that the state, in this situation, is being represented by the Department of Health, which is the entity in charge of the operations by MSH. She said she is also under the impression that the state is making strides toward more community-based care and less institutionalization—but that doesn't align with Whitfield closing its Community Services Division and redirecting funds to inpatient care.
"That's going completely backwards from where we started," Dunaway said.
In a formal response to the Olmstead decision, the state created the 2001 Mississippi Access to Care (MAC) plan—a comprehensive approach to getting those with mental disabilities back out into the community and helping them live and work in the most integrated setting appropriate for their condition. MAC also recommended implementing a system for tracking the state's mental-health clients, but according to the PEER report, DMH has not done so.
Angela Ladner, executive director at Mississippi Psychiatric Association, said none of Mississippi's attempted plans has truly improved mental-health care delivery in the state and that it would require a complete overhaul.
"Mental-health care in our state is in a state of chaos right now," Ladner said. "There are a lot of providers and entities that are vested in the outcome, but there truly is no strategic approach that is coordinated and evidence-based to get us where we need to go."
In 2011 the U.S. Department of Justice found Mississippi in violation of Title II of ADA by failing to provide Mississippians mental-health care in the most integrated setting appropriate. The DOJ recommended that the state facilitate more community-based services. In response, DMH requested additional funds for fiscal year 2013, but the funds were not appropriated.
"Until there is a true dialogue, a true designated comprehensive strategic approach to what needs to be done, we're going to remain in chaos. We're going to continue to have lawsuits filed. It's just not helping anyone," Ladner said.
The Legislature did, however, appropriate $10 million for community-based services for fiscal year 2014 and $16.1 million for fiscal year 2015. The money, DMH officials say, was spent increasing community-based mental health services in the state. The budget was spent on things like developing mobile crisis response teams, Programs of Assertive Community Treatment (PACT) teams and adding additional regional crisis beds for individuals with an intellectual or developmental disability (IDD) and 200 waiver slots to the Home and Community Based Waiter to increase services for that community in need.
But Ladner doesn't believe DMH is using the money in the best way to benefit the mentally ill. "The patients are being denied what the money is there to do," Ladner said. "There are many that we have heard that have been dropped into the street, have taken shelter at Stewpot, sometimes just wandering the streets."
"It's abominable," Ladner said.
This 'Crazy' Contract
After deciding community-based care was outside MSH's primary mission, the state hospital entered into a contract in December 2013 with Key Behavioral Essentials, which was operating under the name Guided Steps Healthcare, to take over the operations of Community Services. The company, which originates in Louisiana but also appears to have had locations in Florida and North Carolina, is a privately operated mental health-care provider. Rep. Currie says the company is on the "Do Not Do Business" list in Louisiana. The company's headquarters in New Orleans did not return phone calls to the JFP.
The contract with MSH states Guided Steps was to "ensure a safe, therapeutic and orderly transition of services" for patients of MSH Community Services from Jan. 6 to June 30, 2014. MSH agreed to pay Guided Steps the Medicaid rate for services provided to individuals without insurance up to $45,000.
Because the contract was for less than $50,000, MSH did not have to seek the approval of the Personal Service Contract Review Board, which would have subjected the contract to a set of rules and regulations. The contract itself is hard to follow—and that, McNair said, is by design.
"It's so complicated, and they made it that way on purpose," McNair said.
The PEER report was critical of MSH's decision to employ a private health-care provider to facilitate the transfer of patients in the Community Services Division since a number of community mental-health centers (CMHC)—which provide the services MSH sought—already exist. In the report, PEER notes that the most recent DMH report indicates that the department primarily contracts CMHCs to provide community services in the state.
Kelly from Hinds Behavioral said she doesn't know why MSH entered into the contract with Guided Steps instead of Hinds Behavioral, which has the capacity to take over the services that Community Services delivered.
"State Hospital never asked us to take over their program or the clients although we got the majority of them," Kelly said. "State Hospital should have asked the community mental-health centers because we're already here. We're already doing it. We should have been given at least the option."
In the Rose Isabel Williams Mental Health Reform Act, enacted by Mississippi Legislature in 2011, the state mandated that DMH and the community mental-health centers work together to develop a plan for delivery of mental-health services to the state. But when it comes to contracting a provider to pick up the pieces of MSH's closure, the department decided to privatize.
"Instead, we get this crazy contract. You have to wonder what was behind that," Currie said.
Guided Steps, however, did not have any of its own buildings, vehicles or computers. It also did not have a proof of physical location or a staffing plan that proved they could provide necessary services. In fact, the company did not meet the basic requirements that DMH sets forth for contract such as these.
The executive director, Christopher Key, did not have a master's degree in a mental health or related field as DMH requires, nor did the department verify his credentials. On his application, he indicated he did have the required master's degree. Key was unable to be reached for this story, but he has since resigned as the registered agent for Key Behavioral Essentials as recorded with Mississippi's Secretary of State.
Because Guided Steps did not have necessary resources, MSH agreed to allow the company to use state buildings, equipment and staff that provided an additional benefit to Guided Steps beyond the amount of the contract.
"Essentially, the contract would have allowed Guided Steps to expand its business in the state," the PEER report stated. "PEER believes that this type of contract is not good public policy, because it uses taxpayer dollars to fund private enterprise."
McNair said she has talked to MSH employees who have said the closure and the seemingly mysterious contract with Guided Steps has created a situation that is "much worse than anyone knows."
"What they've done, they sold the patients. They've stepped back and basically given them to this agency nobody knows a thing about," McNair said, relaying something she had been told.
During the course of the PEER investigation, DMH determined that Guided Steps had acted unethically and, due to that, DMH terminated the contract on April 12, 2014. Many people in the mental health community don't understand why MSH and DMH contracted with Guided Steps in the first place, but most are skeptical it has to do with money.
Currie urges people who want the truth to "follow the money," while McNair claims, "It's a payback for somebody I just don't know who."
Costs Not Absorbed
The location of MSH Community Services' former patients isn't the only concern of health advocate Lynn McNair. She also wonders where the employees of Community Services have gone now that MSH only provides inpatient care.
"Where are the employees? They aren't trained to do inpatient work. None of them are qualified for inpatient work," McNair said.
Interestingly, MSH did not fire employees of Community Services in order to reduce costs as they claimed their goal was to do. According to the PEER report, the division employed 53 staffers as of March 4, 2014. MSH could have eliminated positions through what is known as a RIF, or a reduction in force, which would have allowed them to administratively dismiss employees and direct funds to provide additional community services. This would have been in compliance with the Mississippi Access to Care plan.
Instead, "the department chose to transfer the employees to MSH acute inpatient care."
The PEER report also states that by keeping the employees of Community Services, but closing the division, they eliminated the services "but retained the costs associated with its staff, did not improve its financial position, and the department could not use those resources to move toward providing additional community-based services."
When it comes to the Department of Mental Health, Currie has "never seen anyone be a master of deception with a budget like them," she said.
Ladner said this illustrates exactly her frustrations with the state of mental health care in Mississippi.
"My concern has been that over the course of numerous years we've seen a lot of closures and changes, but we really haven't been given any rationale or seen any improvement based on those closures," Ladner said.
Employees contacted by the JFP were unwilling to go on record regarding their transfer, but the PEER report stated that employees received little communication regarding the elimination of their Community Services positions and whether positions in inpatient care at Whitfield suited their backgrounds and experience.
"Where's the accountability in that? There is none. And the Legislature should be ashamed they let this continue year after year after year without asking the appropriate questions, and now you've got the elected officials that are members of PEER asking the questions that should have been asked by the appropriations committee and the heads and the leaders that are making these decisions.
"It's just been an injustice," Ladner said.
An Excerpt of the Response from the Department of Mental Health to PEER:
"DMH allocates its resources for community mental health services to providers whose primary mission is to provide community services, not inpatient acute care. As MSH's general fund appropriation declined, DMH directed MSH to live within its means, and that included a refocus on MSH's core mission of inpatient acute mental health services. Transition of the individuals CSD serves to other community providers, redirecting CSD resources back into hospital operations, and movement of CSD staff to needed and hard-to-fill positions at the hospital were necessary outcomes of that refocus. Also, the Department of Finance and Administration had indicated the rent charged for CSD facilities may be increasing from a nominal $10 total per year, to $12 per square foot per year (the Capital Facilities customary rate) and the individuals they served. No money was 'saved' by the closure of the CSD; rather, the closure of CSD allowed MSH to reduce the cost of their current operations in order to live within their appropriation.
"DMH and MSH were disappointed that PEER included in the draft report certain editorial comments disparaging DMH and MSH staff motives and commitment toward the individuals we serve. Such opinions and comments are not in keeping with what should be a factual and qualitative audit. PEER began its review of the CSD's closure in the midst of the transition process. Because of this, DMH and MSH believe some opinions were mistakenly clouded by the fears of transitioning employees and advocates unconnected with the transition process. In some instances, PEER staff questioned actions as they were being conducted and planned, rather than evaluating and reviewing those actions after the fact. As a result of the timing of this review, DMH and MSH staff were required to direct an inordinate amount of time and staff resources toward answering PEER staff inquiries, rather than properly directing those resources toward the task at hand."
—Department of Mental Health Executive Director, Edwin C. LeGrand
'Most Integrated Setting,' Defined
The U.S. Department of Justice defends "the most integrated setting" as one that provides individuals with disabilities "opportunities to live, work, and receive services in the greater community, like individuals without disabilities. Integrated settings are located in mainstream society; offer access to community activities and opportunities at times, frequencies and with persons of an individual's choosing; afford individuals choice in their daily life activities; and, provide individuals with disabilities the opportunity to interact with non-disabled persons to the fullest extent possible."
What is Mississippi State Hospital Community Services?
The Community Services Division of MSH started serving patients with mental illness out in the community in 1986. This was so that those patients could remain outside of institutions and maintain a better quality of life.
Support and Therapeutic Services
Case management
Nursing
Psycho-educational counseling
Transportation
Psychosocial rehabilitation
Community living
Community integration
Psychiatric medication
Community Living Services
Villa Hope—A 15-bed group home
Crossroads—A 10-bed group home
MICARE (Mental Illness and Chemically Addicted Recovery Environment)—A transitional substance abuse rehabilitation and treatment home
Community Integration Program
Served patients who received services from MSH inpatient services or Jaquith Nursing Home with day and overnight services.
Jimmy Stubbs House
Also known as Project for Assistance and Transition from Homelessness (PATH). A case management program for the homeless and mentally ill.
Extensive outreach
Psychiatric medication monitoring
Case management services
Drop-in services: laundry and bathing facilities and referral and information services
Source: PEER report






Comments